|
Clinical details:
Definition
Recurrent Respiratory Papillomatosis (RRP) is characterised by the growth of papillomas (wart like lesions) in the respiratory tract (larynx, trachea and rarely lungs) which have a propensity to recur after removal. Although RRP is the most common benign neoplasm of the airway it is still a rare disease with an estimated incidence in the USA of 4.3 per 100,000 children
Clinical Presentations
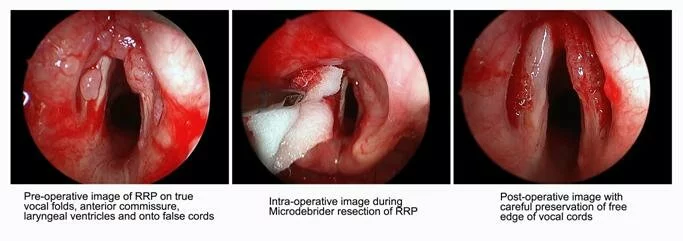
Symptoms usually appear in children 2 to 4 years of age with 25% presenting in infancy. Symptoms reflect the site of involvement with the laryngeal area being most common. The wart like lesions have a predilection for anatomic sites where ciliated and squamous epithelium come together; common sites in the larynx are the true vocal cords, false cords and the laryngeal surface of the epiglottis (Figure ). Children usually present with hoarseness, croupy cough, weak cry, dysphonia / aphonia, and chronic cough. The hallmark of RRP in children is the triad of hoarseness, stridor and respiratory distress. Some children will present in acute distress and require urgent management by the Paediatric Airway team.
Causes
RRP is caused by the human papilloma virus (HPV). The HPV targets epithelial cells and can exist within its host both as an active or latent virus. HPV is a widespread virus with many in the population having genital warts or even asymptomatic HPV. RRP is a rare manifestation. The same HPV virus is associated with cervical cancer in females and is now targeted by a bivalent vaccine in the UK for girls aged 12-13 years.
Vertical transmission of the human papilloma virus (HPV) probably occurs at birth as the newborn passes through an infected birth canal. Two thirds of mothers of children with RRP are positive for genital warts compared to The replicating HPV, most commonly types 6 and 11 and less commonly type 16 or 18, causes the wart-like overgrowths of squamous epithelial cells. The papillomata are multiple projections each with a connective tissue stalk covered by well differentiated stratified squamous epithelium. Viral genome is detectable in surrounding normal appearing tissue suggesting that the infection is more widespread than is clinically apparent. This explains why treatment is so frustrating with recurrences coming after seemingly complete removal.
Diagnosis and investigations (reference 2)
The hallmark of RRP in children is the triad of hoarseness, stridor and respiratory distress.
The diagnosis can be made by visual inspection at laryngoscopy or bronchoscopy (Figure) and confirmed by biopsy. HPV subtyping may be useful in predicting aggressiveness of disease. Type 11 is more likely associated with need for a tracheostomy and types 11, 16 and 18 have a higher oncogenic potential.
Course
During childhood the pattern is typically of papillomas recurring early after removal during periods of activity interspersed with more quiescent periods. The disease, for unknown reasons, usually enters remission when puberty is reached.
Rarely, spontaneous malignant transformation of benign papillomas into squamous cell carcinomas occurs (in
While the papillomas are recurrent in the majority of cases they remain isolated to the larynx and immediate subglottic area. However, between 6 and 12% of cases spread occurs to the distal trachea and in a smaller number this involves the lung tissue. Tracheostomy is associated with tracheobronchial seeding and spread. When the lung papillomata grow they both obstruct airways and destroy tissue resulting in multiple nodular and cystic lesions which can be seen on CT scan. The lesions enlarge and cavitate over time, destroying healthy lung tissue. Although there is little published literature regarding pulmonary RRP it has been considered to be associated with a poor prognosis (reference 3).
Treatment
No single treatment modality has been shown to be effective in eradication of RRP. The current standard of care is surgical therapy with a goal of complete removal of papillomas and preservation of normal structures. Surgical management is aimed at maintaining airway patency, improving voice quality and facilitating remission.
Surgery: Newly diagnosed children with RRP warrant a substantial time commitment on the part of the Paediatric Otolaryngologist (ENT surgeon) and health-care team. Younger children may require surgical debulking initially on a two weekly basis. Tracheostomy should be avoided if possible. CO2 laser vaporization of papillomas can be performed using direct laryngoscopy and a surgical microscope. However, the microdebrider technique for shaving laryngeal papillomas is associated with improved voice outcomes (reference 4). Surgical resection for the rare isolated lung disease may be possible.
Adjuvant therapy (reference 5,6): aims to reduce the frequency that surgical debulking is required. There are no large RCTs showing sustained benefit from any adjuvant therapy and there are no standard criteria for adding adjuvant therapy. Some recommend that it should be started if surgery is needed more than 4-5 times per year. Because pulmonary metastasis from RRP (demonstrated by CT Scan) carries a poor prognosis often with malignant transformation more aggressive adjuvant therapy has been recommended
Interferon (a-2-ß) has occasionally produced dramatic results, but with dose reduction or cessation exuberant regrowth can occur.
Antiviral therapies are typically drugs that inhibit viral nucleic acid synthesis including acyclovir and riboviron. Potentially new antiviral therapies are under evaluation (eg intralesional injection of cidofovir). New improved formulations of Interferon and cidofovir may soon become available.
At present there are too few large well designed randomized control trials to be able to say whether adjuvant antiviral therapy for RRP is beneficial (see reference 4)
Numerous other medications are currently under investigation, including the Epidermal Growth Factor receptor inhibitors such as Celebrex. The RRP task force meet twice yearly in the USA to review new treatments and discuss future research strategies. Recent advances using ‘virus like particles’ to develop vaccines now allow strategies to be put in place for primary prevention. A quadrivalent vaccine against HPV serotypes 6, 11, 16 and 18 offers the possibility of reducing or eventually eradicating the disease (such as Gardasil vaccine used in Canada). Some national vaccination programmes for the prevention of HPV are using bivalent vaccines which do not cover serotypes 6 and 11 which are most associated with RRP (such as Cervarix vaccine used in UK).
|
|
Useful references:
Epidemiology of juvenile onset recurrent respiratory papillomatosis derived from a population level national database."
|
Campisi, P. and C. J. W. Group (2010).
|
The Laryngoscope 9999(999A): NA.
.
|
American Society of Pediatric Otolarngology Member’s experience with recurrent respiratory papillomatosis and the use of adjuvant therapy.
|
S Schraff et al.
|
Arch Otolaryngology Head Neck Surg. 2004; 130: 1039-1042
|
Diagnosis and management of pulmonary metastasis from recurrent respiratory papillomatosis.
|
RD Silver et al.
|
Otolarngol Head Neck Surg 2003; 129: 622-629.
|
Voice outcomes following repeated surgical resection of laryngeal papillomata in children
|
T. Holler et al
|
Otolaryngology - Head and Neck Surgery, Volume 141, Issue 4, Pages 522-526
|
Current status of antiviral therapy for juvenile onset recurrent respiratory papillomatosis
|
Kimberlin DW
|
Antiviral Research 2004; 63: 141-151
|
Adjuvant antiviral therapy for recurrent respiratory papillomatosis
|
Chadha NK, James A.
|
Cochrane Database of Systematic Reviews 2010, Issue 1
|
Web links:
http://www.rrpwebsite.org/
Download this text as a .PDF HERE
|

